Need Help Calculating Your Organizations Prior Authorizations Burden, Get our downloadable spreadsheet.
“How big is your organization’s prior authorizations burden?” More often than not, when I ask this of patient access teams at medical practices, hospitals, and health systems, there is a long pause followed by a “we don’t know.” If you find yourself in this position, you are not alone. A few organizations have been able to properly quantify their prior authorization problem because the workflows are so fragmented, manual, and siloed across multiple functional areas. We’ve spent a decade carefully listening, distilling, and characterizing all the various prior authorization workflows across organizations and want to share some thoughts on how to quantify not only the extent of the problem but also how to focus on where to start. As a former academic healthcare outcomes researcher, – Peter Drucker says, “You can’t manage what you don’t measure.”
Who’s doing what part of the prior authorization? Part of the difficulty in quantifying the prior authorizations burden lies in the hyper-fragmented and highly dispersed nature of the workflows themselves. At some organizations, the initiation or submission of prior authorizations is done in ambulatory clinics, but verifications for the facility are done by a central authorization team. With others, it is highly centralized across the organization by a large central team. Additional challenges arise when the initial submissions are dependent on independent community provider offices that refer in cases that are frequently on different EMRs that don’t talk to each other. Much of these workflows are dependent on faxes, emails, and phone calls.
How do you begin to estimate something that is so manual? So many organizations struggle with how to quantify exactly how much time is spent on prior authorizations by their staff. Because over 80% of today’s prior authorization workflows require manual processing (fax forms, phone calls, typing into web portals), it can be a challenge to come up with a number.
Over the years, we have spent a considerable amount of time working with patient access teams to estimate the amount of staff time that various prior authorization workflows take, and we typically recommend this as a good way to begin formulating some initial estimates of your prior authorizations burden. Here are some of the basic inputs that we find useful in helping to quantify current staffing requirements:
- Estimated volumes of monthly/annual prior authorization transactions (can further be broken down into specific service types or service areas depending on your organizational needs)
- Diagnostic Imaging
- Surgeries/procedures
- Chemo/Infusion therapy
- Medications
- Notice of Admissions
- PT/OT
- DMEs
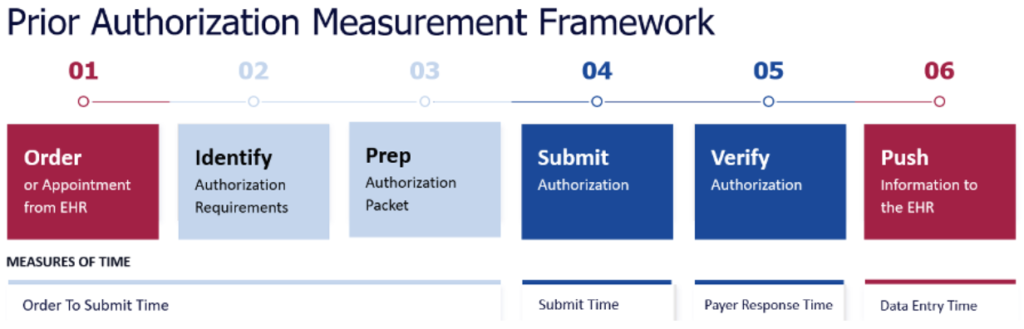
- Estimated average time spent on processing particular prior authorizations by workflow type (fax forms, clinical survey-based web portals, standard web portals, etc). Estimates of processing times should be inclusive of the following: gathering info from EHR, identifying requirements, submitting prior authorizations, checking on status to verify prior authorizations, and inputting data back into EHRs.
Although estimated times can vary by organization, authorization modality (fax, web portal), payer, and individual staff member, our experience has been that the average staff processing time per authorization is generally between 16-25 minutes. According to the most recent CAQH Index report, the average time for prior authorizations is 20 minutes.
- What is the number of current staff working on processing prior authorizations? This can be somewhat tricky to come up with a headcount depending on whether staff spend the majority of their daily time working primarily on prior authorizations or in conjunction with other front-end activities (eligibility verification, scheduling, etc.). For some organizations, it can be relatively straightforward with a central authorization team, and for others distributed across various clinics.
With these basic estimates in place, you can begin to understand your organization’s overall staffing requirement needed to process current prior authorization volumes. It’s also a good way to understand if your teams are indeed understaffed (particularly with worsening staffing shortages) to reasonably handle increasing volumes. With this data, we can begin to estimate not only the average authorizations/FTE/day, average annual authorizations/FTE, and ultimately what total organizational staffing costs look like.
An additional methodology for quantifying the prior authorizations burden beyond staff time calculations is denied claims payments related to prior authorization errors/issues. Metrics such as first-pass authorization denial rates can be useful to identify the scope of the financial impact that can be quite significant and variable depending on your organization’s revenue cycle processes and performance. Much of the denials attributable to prior authorizations may be avoidable errors and write-offs due to front-end activities (e.g. putting in correct authorization tracking numbers into claims).
If your organization has access to 835/837 via your clearinghouse provider, you can get an estimate of not only the total volumes (what volume of claims had the prior authorization number populated on 837s), as well as what the volume of prior authorization denials are on 835s, and total denied dollar impact. Depending on the service lines and the performance of your revenue cycle teams this can add up to a significant financial burden above and beyond your staff’s time processing authorization on the front-end.
Let us help you calculate your organization’s prior authorizations burden with this FREE downloadable spreadsheet.