Guide
Comparing Manual & Automated Prior Authorization Approaches
How to reduce staff time, cost, and avoidable denials.
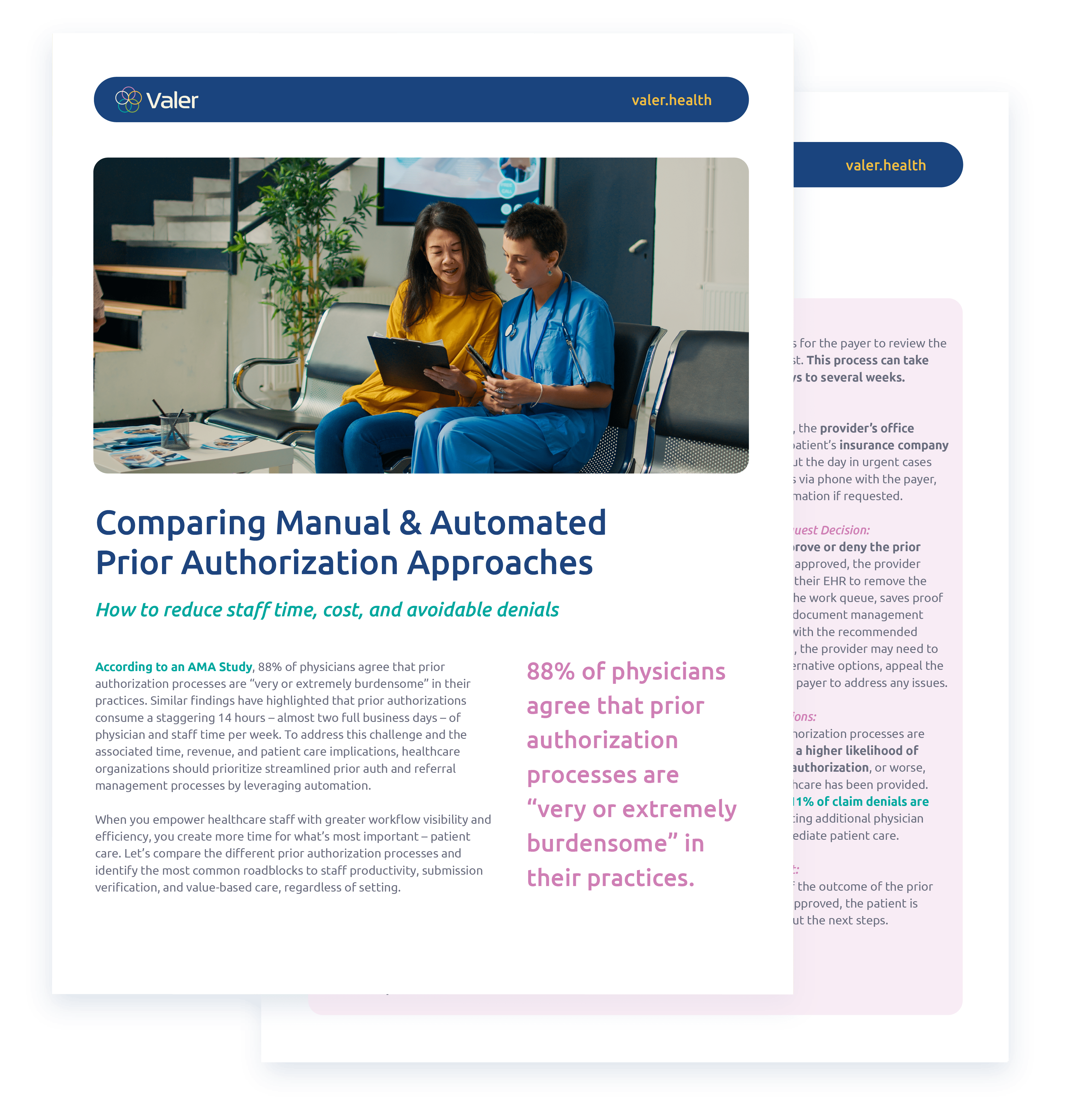
Prior authorization is a significant burden in healthcare, with 88% of physicians finding the process “very or extremely burdensome,” according to a recent AMA study. It consumes nearly 14 hours of physician and staff time per week, directly impacting revenue and patient care.
Automated prior authorization can revolutionize your workflow, reducing manual errors and freeing up valuable time for patient care. But how do manual and automated approaches really compare, and is the investment in automated solutions worth it for your care setting?
Key Insights from Our Guide: A High-Level Look

Evaluation of Medical Necessity
Both manual and automated prior authorization methods start with assessing the patient’s medical condition.

Insurance Verification
Manual processes involve time-consuming insurance checks and wait times, while automated solutions offer real-time eligibility verification.

Documentation & Submission
Manual prior authorization form completion and submission are prone to errors, whereas automated systems pre-populate and submit forms electronically, minimizing mistakes and costly denials.

Approval & Follow-Up
Manual status checks require extra time and resources. Automated solutions continuously track and update the status, ensuring timely decisions and fewer denials.

Recordkeeping
Automated solutions maintain comprehensive records for reporting and streamlining administrative tasks. This means better insights into approvals, denials, and communications.
Why should you automate your prior authorization process?
It’s time to leave your manual prior authorization process behind. Automated prior authorization systems minimize data entry errors and streamline the entire process. They also free up staff to focus on patient care instead of paperwork, giving physicians and support staff valuable time back in their day. Lastly, automated prior authorization solutions improve efficiency by providing real-time updates and integrating with EHR solutions, enhancing workflow visibility and productivity.
Get the Full Comparison
Access our detailed guide to understand the complete breakdown of manual vs. automated prior authorization processes. Learn how automation can help you achieve better outcomes, lower costs, and improve patient care.



